Anesthesia for Tracheal Stent Placement
July 22, 2025 · Dogs

Patient: “Beau” Juilerat (MR# 278941) - 5 yo MN Yorkshire Terrier – 6 kg
Presenting complaint: intermittent coughing and dyspnea, possible tracheal mass
Case summary
Beau presented to the AVES Internal Medicine Service on 6/5/25 for intermittent coughing, dyspnea and evaluation of a possible tracheal mass noted on thoracic radiographs taken by his primary veterinarian.
Beau was anesthetized for diagnostic imaging. CT of his neck and chest revealed tracheal malformation and collapse with severe narrowing of portions of his trachea. Tracheoscopy was then performed and confirmed a diagnosis of tracheal malformation and collapse.
Following tracheoscopy, an intraluminal tracheal stent was placed under fluoroscopic guidance. Correct placement of the stent and resolution of Beau’s previous tracheal collapse was confirmed with post-procedure thoracic radiographs.
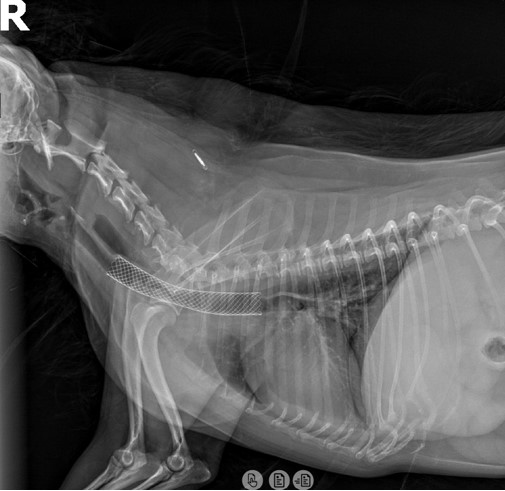
*Image above shows post-procedure thoracic radiographs confirming placement of intraluminal stent in the cervical and thoracic trachea. Expansion of the previously collapsed portion of trachea is noted.
Beau experienced no complications and recovery from anesthesia was uneventful. His breathing was noted to be improved from prior to tracheal stent placement. He had no immediate post-procedural complications and was discharged from the hospital the following day.
Anesthetic considerations for tracheal collapse and tracheal stent placement
Patients with tracheal collapse present a variety of unique anesthetic challenges. The trachea is the primary airway within the neck and chest responsible for delivering oxygen to the lungs with each breath. In the event it becomes partially or completely obstructed during collapse, the patient may be unable to deliver oxygen to the lungs and be at risk of hypoxemia. Severe or prolonged hypoxemia can cause immediate and/or serious complications including organ injury, brain injury and death. Appropriate pre-anesthetic sedation, anesthetic induction and airway management are fundamental to successful patient outcomes. In some patients, portions of the trachea may still collapse during parts of the breathing cycle despite endotracheal intubation. Application of a special breathing technique known as positive end-expiratory pressure (PEEP) can help prevent tracheal collapse in these patients. Beau’s anesthesia for CT of his neck and chest was uneventful with no occurrences of airway obstruction.
Placement of a tracheal stent poses several additional anesthetic challenges. The same anesthetic considerations for patients with tracheal collapse apply but with the addition of procedure-specific obstacles. The primary obstacle is patients must be extubated in order to perform the stent placement procedure.
This presents the following challenges:
Patient airway is not protected from aspiration in the event regurgitation occurs during the procedure. Beau was administered metoclopramide peri-anesthetically to reduce the risk of regurgitation. Diligent monitoring of the upper airway and oral suctioning as needed were also performed.
Tracheal collapse and airway obstruction may occur once the patient is extubated. The endotracheal tube is often used to support or bypass areas of tracheal collapse. With the tube removed there is a risk collapsed areas may obstruct the airway. Fortunately, airway obstruction did not occur during Beau’s anesthesia when his endotracheal tube was removed. However, the anesthesia team was prepared to address this complication had it occurred.
Anesthesia cannot be maintained using a volatile anesthetic. During the maintenance phase of anesthesia, the vast majority of veterinary patients are kept anesthetized using a vaporized anesthetic drug (isoflurane or sevoflurane) delivered via a breathing circuit. Vaporized anesthetics are delivered in 100% oxygen through the endotracheal tube to the patient’s lungs where they are absorbed into the bloodstream across thin capillaries. Without an endotracheal tube in place, volatile anesthetics cannot be used to maintain anesthesia and IV anesthetics must be utilized instead. During his stent placement, Beau’s anesthesia was maintained using an IV medication called alfaxalone delivered with a specialized pump at a precise dose.
Oxygen cannot be administered directly to the patient’s lungs. The endotracheal tube is used to deliver 100% oxygen to the patient’s lungs to prevent hypoxemia during anesthesia. Without this, another means of delivering oxygen to the patient’s respiratory system must be applied. While there are different methods to accomplish this, in Beau’s case, specialized nasal cannulas were passed through his nostrils and placed in the nasopharynx to deliver oxygen to the upper airway. This method does not deliver the same amount of oxygen to the lungs as an endotracheal tube, but it is effective in preventing hypoxemia. Beau experienced no episodes of hypoxemia during anesthesia.
Closing remark
Beau’s anesthesia and tracheal stent procedure were overall uneventful thanks to the skill and experience of the AVES Internal Medicine and Anesthesia Services. He recovered well from anesthesia, his breathing was immediately improved and he returned home the following day.
